
A broken or fractured tibia can be a painful and debilitating injury, often resulting from high-impact trauma or accidents. As the main bone in your lower leg, the tibia plays a crucial role in supporting your body’s weight and enabling movement. Whether you’re an athlete, an active individual, or simply someone who has experienced a fall, understanding the symptoms, healing stages, and when to seek medical help is essential for a smooth recovery.
In this guide, we’ll walk you through the key signs of a tibia fracture, how the bone heals over time, and the steps to take if you suspect a break. By recognizing the right course of action, you can ensure the best possible outcome for your leg’s healing journey.
At Academy Orthopedics, we specialize in treating a wide range of knee conditions, including tibia fractures, ligament injuries, cartilage damage, patellar issues, and osteoarthritis. Our expert orthopedic team offers tailored treatment plans to help you heal effectively and return to your daily activities with confidence. Call us at (770) 271-9857 or book your consultation online now.
👉Also Read: Outpatient Knee Surgery: A Game Changer for Faster Recovery and Better Outcomes
Recognizing Symptoms of a Broken Tibia
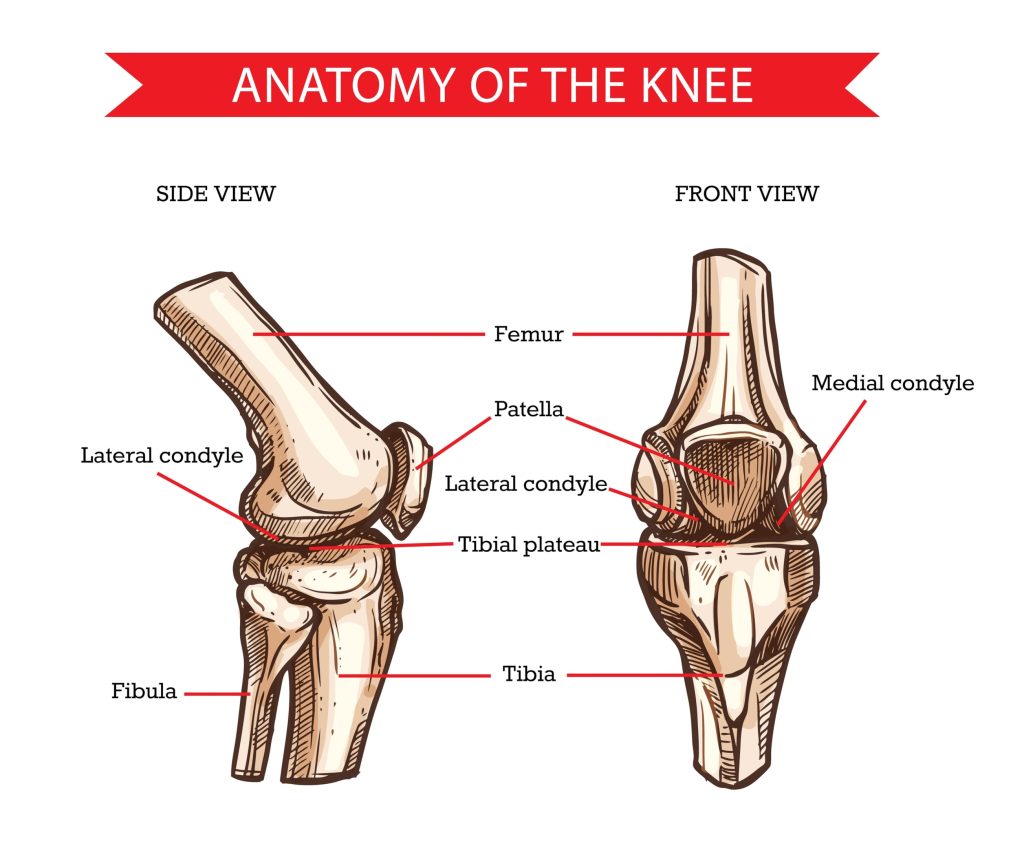
Identifying the symptoms of a broken tibia and fibula early helps ensure timely medical treatment and prevent further complications. The tibia, along with the fibula, forms the two lower leg bones and is one of the most commonly fractured long bones in the body. When the tibia breaks, symptoms can be immediate or delayed, each revealing important details about the injury.
Immediate Signs
Immediate signs of a tibia fracture often include severe pain, making it challenging to walk or put any weight on the affected leg. This pain is usually the first symptom noticed and can be accompanied by visible instability or deformity in the leg. In many cases, the leg may also exhibit extreme bruising and swelling, adding to the visible indicators of a broken bone.
Delayed Symptoms
Delayed symptoms of a tibia fracture can be just as telling as the immediate ones. Swelling and bruising around the fracture site often become more pronounced in the days following the injury. Additionally, tenderness can develop over time, signaling ongoing injury and inflammation.
Tracking these symptoms provides critical information about the fracture’s progression and the body’s healing response. Neglecting delayed symptoms can result in complications, so remain vigilant and seek medical advice if these signs continue.
Types of Tibia Fractures and Their Impact on Recovery
Tibia fractures come in various forms, each impacting the recovery process differently. Knowing the type of fracture is important because it affects the treatment approach and healing timeline. Tibia fractures can be categorized based on their location and the pattern of the break, which helps in devising an effective treatment plan.
Common types of tibia fractures include:
- Transverse fractures, which feature a horizontal break
- Comminuted fractures, where the bone is shattered into multiple pieces
- Oblique fractures, which present an angled line across the bone
Each type has distinct characteristics and implications for recovery. For instance, transverse fractures are generally more stable compared to oblique fractures.
Transverse and Oblique Fractures
Transverse fracture, characterized by a horizontal break, and oblique fracture, featuring an angled line, are common types of tibia fractures. These fractures differ in stability, with transverse fracture generally being more stable compared to oblique fractures.
The treatment for these displaced fractures sometimes involves immobilization using casts or braces to ensure proper alignment and stability during the healing process. But more commonly in adults, it involves surgical repair.
Comminuted and Spiral Fractures
Comminuted fractures, where the bone shatters into three or more pieces, and spiral fractures, caused by a twisting force and wrapping around the bone, are more complex types of tibia fractures. These fractures are highly unstable and require careful management, often involving surgical intervention to stabilize the bone fragments and facilitate proper healing.
The complexity of these fractures necessitates a detailed and personalized treatment plan to ensure successful recovery.
Causes of Tibia Fractures
Fractures of tibia and fibula can occur due to a wide range of incidents, broadly classified into high-energy and low-energy injuries. Identifying the cause of the fracture is crucial for effective treatment and future injury prevention.
High-Energy Injuries
High-energy injuries, such as those resulting from motorcycle crashes or severe car accidents, are major contributors to tibia fractures, particularly in the proximal region (towards the knee). These injuries often lead to complex fractures involving multiple bone breaks and significant soft tissue damage. Immediate and intensive medical intervention is typically required, which may involve surgical procedures and a lengthy recovery period. The severity of the impact can complicate the healing process, making prompt treatment and ongoing medical care critical.
Low-Energy Injuries
Low-energy injuries are often the result of falls or minor trauma, particularly in older adults who may have decreased bone density. While these fractures may appear less severe, they can still be significant, especially in individuals with pre-existing bone conditions, such as osteoporosis. Recognizing the increased risk in older populations is essential for early intervention, preventing complications, and ensuring optimal healing. Timely treatment can help reduce the risk of future fractures and improve long-term outcomes.
Diagnostic Process for Tibia Fractures
Diagnosing tibia fractures accurately is vital for determining the fracture’s extent and type, influencing the treatment plan. This process typically involves gathering a detailed medical history, performing a thorough physical examination, and utilizing various imaging techniques to accurately assess the injury. An accurate diagnosis is essential for effective treatment and successful recovery.
Medical History and Examination
During the diagnostic process, healthcare providers gather detailed information about how the injury occurred and assess the patient’s overall medical history. The physical examination includes checking the condition of soft tissues around the knee joint, looking for bruising, swelling, and any open wounds.
Evaluating nerve function and blood supply ensures no additional damage has occurred.
Imaging Tests
Imaging tests are crucial in diagnosing a fractured tibia. X-rays are typically the first step, providing clear images of the bone structure and the location of the fracture. CT scans offer more detailed views, which are particularly useful for assessing the severity and complexity of the fracture.
MRIs may be used to evaluate any associated soft tissue injuries, ensuring a comprehensive understanding of the injury. Imaging techniques are essential for accurate diagnosis and effective treatment planning.
Emergency Treatment for a Broken Tibia
Emergency treatment for a broken tibia is crucial to prevent further complications and ensure proper healing. Immediate intervention is crucial, especially for open fractures or heavy bleeding. Early treatment focuses on stabilizing the injury, providing pain relief, and preventing infections and complications such as compartment syndrome.
The first step in emergency care is stabilizing the injured leg, often with splints to minimize movement and pain. Pain relief is managed through medication to ease discomfort until professional medical care is available.
Infection prevention is critical for open fractures, requiring thorough cleansing to reduce the risk of bone infections. Monitoring for signs of compartment syndrome, a serious complication characterized by increased pressure in muscle compartments, is also essential.
Stabilization and Pain Relief
Stabilizing a broken tibia immediately after the injury is essential to prevent further damage and provide pain relief. Using a splint can effectively immobilize the leg, minimizing movement and discomfort until professional medical care is available. Pain relief can be managed through medications administered at the scene or in an emergency setting.
Stabilizing the leg eases pain and prevents further complications, setting up for effective treatment and recovery.
Infection Prevention and Compartment Syndrome
Infection prevention is a critical aspect of emergency treatment for open tibia fractures. These fractures require thorough cleansing to reduce the risk of infection, which is a common concern in such cases.
Monitoring for compartment syndrome is crucial, as it can develop rapidly and requires immediate intervention. Compartment syndrome occurs when swelling compresses blood vessels, leading to reduced blood flow to muscles, and requires timely treatment to prevent severe outcomes.
Healing Stages of a Tibia Fracture
Healing from a tibia fracture is a multi-phase journey that includes inflammation, repair, and remodeling. Knowing these stages helps manage recovery expectations and ensure proper care. Typically, the healing process spans four to six months, progressing through several key phases.
Initially, the body reacts to the injury by creating a hematoma at the fracture site, which forms a blood clot and initiates the healing process. The intermediate phase involves the formation of a soft callus, which later hardens to provide provisional stability.
Finally, the remodeling phase reshapes and strengthens the bone, often requiring physical therapy to restore strength and flexibility.
Initial Healing Phase
The initial phase of healing begins immediately after the fracture occurs. The body reacts by forming a hematoma at the fracture site, which helps prevent further damage and initiates the healing process.
Nonsurgical treatments during this phase typically include casting, bracing, and restricting motion and weight-bearing activities to stabilize the fracture and allow the soft tissues to recover. Proper care during this phase sets the foundation for effective recovery.
Intermediate Healing Phase
In the intermediate phase, the body forms a soft callus around the fracture site, which gradually hardens and begins to mineralize, providing more stability to the bone. This phase also involves the formation of granulation tissue within two weeks, which facilitates the beginning of new bone formation and provisional stability.
These processes are critical for transitioning to physical therapy and active rehabilitation.
Final Healing and Rehabilitation
The final stage of healing involves bone remodeling, where the newly formed bone is reshaped and strengthened through mechanical stress over several months. Rehabilitation during this phase is crucial and includes physical therapy to regain strength, flexibility, and function.
Strengthening exercises enhance physical fitness and are vital for returning to normal activities after healing.
Treatment Options for Tibia Fractures

The treatment for a tibia fracture is determined by several factors, including the type and severity of the fracture, the patient’s age and overall health, and the specific location of the break. Broadly, treatment options can be categorized into nonsurgical and surgical approaches, each with its own set of procedures, benefits, and recovery timelines. Choosing the right treatment is crucial for optimal healing and minimizing long-term complications.
Nonsurgical Treatments
Nonsurgical treatments are typically recommended for stable fractures, where the bone ends remain well-aligned and do not require intervention to realign the bones. These approaches are ideal for less severe fractures, where the risk of complications is minimal, and the healing process can occur naturally with proper stabilization.
Common nonsurgical treatments include:
- Casting – A plaster or fiberglass cast is applied to immobilize the leg and protect the bone while it heals. This approach is most effective for fractures that are stable and aligned, where movement must be limited to ensure proper healing.
- Bracing – For some fractures, a brace may be used instead of a cast. This option allows for more flexibility while still stabilizing the bone. Bracing is typically used for fractures that are less severe but still require support during the recovery period.
- Walking Boots – A walking boot is used when the patient can bear weight on the leg, but still requires support and protection to avoid further injury. This treatment is generally used for less complex fractures where some mobility is possible during recovery.
The goal of nonsurgical treatments is to allow the bone to heal naturally by keeping the fracture stable and restricting movement. This process can take several weeks to a few months, depending on the nature of the fracture and the patient’s overall health.
Surgical Treatments
Surgical treatments are typically required for more complex fractures, including those that are unstable, displaced, or associated with significant soft tissue damage. These fractures may not heal properly with nonsurgical methods and often require surgery to restore proper alignment, stabilize the bone, and prevent long-term complications.
Common surgical options include:
- Internal Fixation – This is the most common surgical procedure for tibia fractures. In internal fixation, the surgeon uses metal rods, plates, and screws to hold the bone fragments in place while the bone heals. This method allows for better alignment and faster healing than nonsurgical approaches, especially for displaced or comminuted fractures.
- External Fixation – In cases where the fracture is open (the bone is exposed through the skin) or the soft tissue is severely damaged, an external fixation device may be used. This device consists of pins inserted into the bone, which are then connected to an external frame. External fixation is typically used in emergencies or for fractures that are difficult to stabilize with internal fixation.
- Intramedullary Nailing (IMN) – This technique involves inserting a metal rod (nail) into the bone’s marrow cavity to stabilize the fracture from the inside. IMN is commonly used for fractures of the tibia shaft and provides a secure and stable environment for healing.
- Bone Grafting – In cases where there is significant bone loss, or if the fracture does not heal properly, a bone graft may be used. This involves transplanting bone tissue (either from the patient or a donor) to stimulate bone growth and promote healing.
Surgical treatments usually require a more extended recovery period than nonsurgical methods, with rehabilitation and physical therapy often being necessary to regain strength, flexibility, and functionality in the leg.
Indicators of Complications in Tibia Fracture Healing
Monitoring for complications during the healing process of a tibia fracture is crucial for ensuring successful recovery. Persistent pain, increased tenderness, and abnormal limb alignment are key indicators that something may be wrong. Early recognition of these signs allows for timely intervention and treatment adjustments.
Compartment syndrome is a serious complication that can occur, characterized by increased pressure within the muscle compartments, which threatens blood supply to the leg muscles and nerves. If any concern for compartment syndrome it is very important to present to the emergency room as quickly as possible. Other potential complications include malalignment of fracture fragments, which can delay healing or lead to nonunion of the bone.
When to Seek Medical Help
Seeking medical help promptly for a tibia fracture is essential to prevent further complications and ensure proper healing. Immediate medical attention is crucial if there is inability to bear weight, loss of sensation, severe pain, or inability to move the leg.
Regular follow-up appointments with healthcare providers are also vital for monitoring the healing process and addressing any potential complications early on. Regular follow-ups ensure proper bone healing and prompt detection and management of issues. This approach helps in achieving a safe and effective recovery.
👉Also Read: Meniscus Tears: The Importance of Treating Them Without Delay
Get Back on Your Feet with Academy Orthopedics: Expert Care for Tibia Fractures – Start Your Healing Journey Today!
At Academy Orthopedics, we’re dedicated to helping you recover with expert care and personalized treatment options. Whether you’re dealing with a minor injury or a complex fracture, our team is here to guide you through the healing process every step of the way. If you suspect a tibia fracture or are facing complications in your recovery, don’t wait—contact Academy Orthopedics today at 770-271-9857 for a comprehensive consultation. Your path to healing starts here.
